I have previously blogged about forearm synostosis HERE. A few important points
1) It uncommon compared to other upper extremity anomalies but is perhaps the most common of the forearm birth differences.
2) It is really well tolerated by most children. Especially because the rest of the upper extremity is typically normal (most importantly, the hand)
3) The function impact depends on a few factors:
The position of the forearm (i.e., how rotated is it)
Whether one arm or both
The child- each child is affected differently
4) It is recognized later than many birth anomalies because it is not immediately obvious.
It is a bony problem and the forearm can look normal. Parents often count fingers and toes but, unless the parent is a congenital hand surgeon, parents do not typically test forearm rotation.
Each of us can “rotate” through our wrists so that it looks like the forearm is rotating. Unless you actually feel feel the forearm, determining rotation can be tough.
Functional limitations may be few and often do not become obvious until the child is required to perform higher- order tasks (often school age or sports).
When is surgery helpful?
Surgery is not typically required but a few factors increase the likelihood of surgery being helpful. First, when both forearms are affected it is more difficult for the child to compensate. And second, when the forearm is fixed in severe rotation (typically palm down/ pronation but can be palm up/ supination).
What is the ‘best’ surgery?
There are two basic concepts for surgery (and only one works).
1) The most appealing to every single parent and every single surgeon- restore rotation of the forearm. That is, take out the bony block and allow the radius and ulna to rotate the forearm. There have been a huge number of techniques attempted but I want to be clear: these surgeries do not work.
2) Position the forearm in a more neutral posture (think clapping position). This allows shoulder motion to help position the hand and is a highly effective surgery. This requires cutting and repositioning the bones. There are two techniques
a) I believe more surgeons are using a technique to cut the bone at the site of the bony fusion (the synostosis). This works but, in my opinion, has a few challenges.
It requires metal pins for approximately 6 weeks while the bone is healing. Pins can sometimes cause problems. Pins are typically removed in the office but occasionally in the operating room.
Like every surgery, there can be complications.
b) A two- stage procedure called osteoclasis. I like and use this procedure with younger kids. Each stage is straightforward. In the first stage, the bones are cut but not moved. This limits the nature of the surgery and the risks. In the second stage, the bones are rotated to the desired position and casted. Healing almost always occurs by 6 weeks. The negative of this surgery is the fact that it is 2 stages but there are many advantages for the right child and the right family.
Here is a great example. The four x-rays capture the deformity and the joining of the bones (again, the formal name is synostosis) near the elbow.
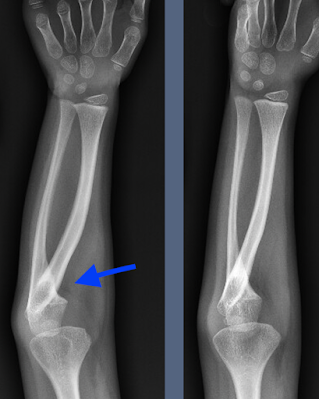 |
| Forearm synostosis. Arrow points to the bony joining bw radius and ulna. |
 |
| Forearm synostosis. Arrow points to the bony joining bw radius and ulna. |
This young patient was treated with a two- stage osteoclasis procedure. Below are a few pictures marking the incisions and the initial x-rays for the first stage. The incisions are quite small (< 1 inch).
| Marked (two dots) planned incision for osteoclasis procedure in which the radius bone is cut |
| Marked (two dots) planned incision for osteoclasis procedure in which the ulna bone is cut |
| After cutting the radius and ulna for forearm synostosis |
| After cutting the radius and ulna for forearm synostosis |
There is not much to share after the second stage (rotation of forearm to the desired position). You might wonder- why not do all in one stage? This is a great question with two answers. Delaying the rotation decreases complications and helps to maintain the new position b/c the bone are ‘sticky’ as they start to heal. That is why no metal (pins) are required.
Thanks for reading,
email: congenitalhand@wustl.edu
Please CLICK HERE to support our research.
Designate my name. Thank you!