The treatment of extra toes and toe syndactyly often involves the hand surgeon given the overlap in treatment strategies between hand and foot. As I have previously blogged, I typically avoid reconstructing toe syndactyly unless it involves the first web space (ie, the great toe). While there are exceptions to this approach, the risks of […]
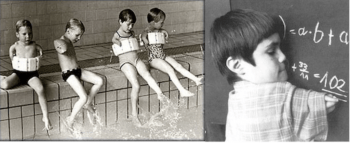
Hand Camp 2023

The St Louis Shriners Hospital began hand camp in 2008 and it has taken place in early autumn each year in Pitosi, Missouri (except during COVID when it was virtual). This year the camp was October 13-15, a bit later than usual and, also, a bit chillier than usual. But the energy and love was […]
Hand Society (ASSH) 2023 Travels
The ASSH Annual Meeting was in Toronto this year. As usual, it was a fabulous meeting and its always great to connect with friends from across North America and the world. There were very good pediatric sessions throughout the week! We had a fantastic Pediatric Hand Study Group (PHSG) meeting. The group continues to grow with a goal […]
Digital Lengthening
Shortened digits are a common concern of parents when their child is born with a difference. For most kids, lengthening does not make sense as it will not improve function or appearance. However, for some kids, the procedure can make a big difference. The most common situation is amniotic constriction band in which digits are […]
Building Community in the Congenital Hand World
There is remarkable value in a medical community. There are a wide variety of such communities, each with important benefits. While this blog will not discuss all such communities, I want to share thoughts on some of these. One very important community is the patient- to- patient community with a sharing of experiences, outcomes, and […]
Bone Lengthening in Olliers Disease
I have been curious about ChatGPT and so I wanted to share an encounter with artificial intelligence. Honestly, I am impressed. The complete response: “Ah, I see. Multiple enchondromatosis, also known as Ollier’s disease, is a rare, non-hereditary skeletal disorder characterized by the presence of multiple benign tumors called enchondromas. Enchondromas are growths of cartilage […]
Hand Camp 2022
I am so excited that we were able to host Hand Camp in 2022. This camp is supported by the St Louis Shriners Hospital and organized by the amazing hand therapy team. We had our first hand camp back in 2008 with only minor interruptions since (COVID). This year we hosted 19 families (including affected […]
Mirror Hand, The Elbow & Ulnar Dimelia
Mirror hand, or ulnar dimelia as it is technically known, is one of the most striking birth differences of the upper extremity (there is also a lower extremity similar condition). There is a duplication of the ulnar half of the forearm and hand. This can present in the hand only (with a normal forearm) or […]
Rare Condition of Patient with 3- arms, Special Relationship

It has been more than 10 years since I first met a special child from Central America. He had a condition which is incredibly rare, with only a few reports ever. You see, Erickson was born with 3- arms. His right side was normal but, on the left, he two arms. The upper one had […]
Cleft Hand vs Symbrachydactyly, Cleft Type
Both cleft hand and symbrachydactyly may present in different ways, which can make it difficult sometimes to understand the difference. Symbrachydactyly presents in 4 types for the hand: cleft type (the point of this post), monodactyly type (only a thumb), short finger type, and peromelic (just nubbins). I have previously posted about symbrachydactyly here, here, […]
Travels: World Pediatric Project, Barbados
WPP The WPP is a wonderful organization that I have worked with for more than 15 years. Based on Richmond, Virginia and Saint Louis, Missouri, it is focused on the global health of kids in many areas including orthopedic surgery. When I first became affiliated, kids with major orthopedic issues came to St Louis for […]
Murderer’s Thumb
Murderer’s thumb is one name for brachydactyly, type D. The is a short, round distal phalanx of the thumb and may be one on side or both. The nail looks wide relative to the overall length of the thumb. Other common names include stub thumb and club thumb (not to be confused with the medical […]
Understanding the Specifics of Upper Extremity Birth Differences, Part 2
It has been far too long since my post on the “Why” of Birth Differences. I apologize and I know at least some of you have been awaiting this post. No excuses but I am now on a new platform and the transition took time. This is Part 2 in which I will review some of the […]
Part 3. Genetic Testing
This is the 3rd in an overview series on congenital differences (i.e., conditions present at birth) of the upper extremity. It might help to review Part 1 (Understanding the ‘Why’) and Part 2 (Specifics of Common Differences) before reading the following but each does stand on their own. My goal in this post is to […]
Syndactyly, Macrodactyly, and Keloid

The treatment of syndactyly is highly successful, no matter the preferred technique. That is the classic technique of Flatt (dorsal commissure flap and zig- zag incisions- ) or graftless techninques or hyalomatrix- all can work. Complications include web creep (maybe not a true complication as it is so commonly seen), wound healing issues, rare infections, […]
Understanding the ‘Why’ of Upper Extremity Birth Differences Part 1
Birth differences of the upper extremity have many different forms/ presentations. These can be a dramatic with a shortened or deviated extremity or very subtle/ mild with slightly short fingers or a subtle lack of muscle development. In my three decades of caring for kids, it has always been clear that our team is truly […]
Forearm Synostosis- Facts and My Approach to Treatment
I have previously blogged about forearm synostosis HERE. A few important points 1) It uncommon compared to other upper extremity anomalies but is perhaps the most common of the forearm birth differences. 2) It is really well tolerated by most children. Especially because the rest of the upper extremity is typically normal (most importantly, the hand) […]
2 Reasons for Less than 5 Fingers
A brief post with lots of pictures and videos on two conditions that may cause less than five fingers. As I have previously written, there are 5 common causes. Parents have given permission. Diagnosis 1. Symbrachydactyly. This patient has a great thumb and nubbins past the metacarpals. However function is excellent. The child will likely […]
2 Common Types of an Uncommon Condition- Symbrachydactyly
When I consider all of the different patients with a birth anomalies that I have the privilege to evaluate and treat, there is no question that symbrachydactyly is the diagnosis most often misnamed or unnamed. Amniotic constriction band is perhaps most commonly given as the incorrect diagnosis for the patients. Symbrachydactyly literally means short, webbed […]
An Unusual Pollicization Procedure
Radial polydactlyly (extra thumb) is a relatively common problem for those of us who treat kids with birth differences/ anomalies of the upper extremity. Please see the following link for previous posts on the topic LINK. Sometimes these can be treated by a “straightforward” procedure with excision of the extra thumb and stabilization of the primary […]
Early Action in Madelungs Deformity
Years ago, I met an 7 year young lady who came to my office with no complaints. Mom brought her even though she had no hand or wrist pain and no functional limitations. The reason for the visit was a strong family history of Madelungs deformity (mom and sister). There was no clinical evidence of […]
Syndactyly as part of a syndrome
Syndactyly is most commonly an isolated finding which we believe is “simply” related to a failure of the cells to regress during development. This failure to regress means that the webspace does not develop ~ the 7th-8th week of gestation. We know that the apical ectodermal ridge is involved and signaling mechanisms including FGF-8. This […]
Tight First Webspace
The space between the thumb and index (pointer) finger is crucial for function. We say that the thumb accounts for 40% of hand function – much of that function is related to grasping large objects in this ‘first webspace’. The thumb-index webspace, or as it is also called- the first webspace, can be tight or […]
Pollicization Long Term
Hello all. I want to share a good result in a challenging pollicization procedure. This patient has radial longitudinal deficiency with a poor, very limited thumb (we call it type 4 hypoplastic thumb). The decision was made to excise the thumb and create a new one with the index finger (e.g., the pollicization procedure). We […]
Radial polydactyly- progress and patient follow up
I have shared my thoughts on radial polydactyly (extra thumb) a number of times- those other posts can be found at https://bit.ly/3emosGU. Radial polydactyly is a common diagnosis for those children with birth differences but each child and each extra thumb is also very different. This makes comparing children difficult and results are limited in the […]
The Elbow in Birth Differences of the Upper Extremity
The elbow is not commonly discussed around the topic of birth differences of the upper extremity. We discuss fingers, wrist, and forearm most commonly. The shoulder is also occasionally involved but much less so compared even to the elbow. My goal in this blog post is to highlight some of the birth differences that may […]
Congenital Differences- Timing of Intervention in the era of COVID-19
March 28, 2020 We are in an unprecedented time. COVID-19, the coronavirus which began in Wuhan Province in China in late 2019, has impacted our world in many ways. Medical centers in the US and Europe are in a time of crisis as they prepare for or are in the midst of the pandemic. In […]
Radial Deficiency Outcome
Radial deficiency (or radial longitudinal deficiency, RLD) is one of the most challenging conditions that I treat. We classify patients with RLD based on their bone development but that does not capture the underlying muscle and joint abnormalities. Reports on treatment including surgery have been mixed and that has led hospitals and doctors to have […]
Syndactyly: The Type Matters.
Syndactyly, simply put, means joined fingers. However, there are a number of different types including:– cutaneous (or simple)- only a skin connection– Complex- with a bony connection– Complicated- with an associated syndrome– Partial vs complete (whether part way or completely to tip of finger).– Complex polysyndactyly. That is, extra bones and bony connections. The partial […]
Two different thumb birth differences
The thumb is our most important digit. In the adult, we estimate that it affects about 40% of hand function. So, a thumb that is not fully or normally developed may really affect our abilities- whether that be strength, motion, dexterity, etc. I have written a number of posts (See HERE) about the thumb but […]
Recurrent Syndactyly
Syndactyly is the abnormal connection between fingers- typically skin connection but sometimes bony connection (called complex). I have written much about it HERE. There is also information on the internet including some basic information on Wikipedia, NIH, and numerous hospital websites. While syndactyly is one of the most common congenital upper extremity diagnoses, treatment is not perfect and ‘failures’ […]
Cleft Hand: Beyond the Basics
I have posted numerous times on cleft hand. (See other posts.) In my world, this is a still an unusual diagnosis and can be challenging as each child is somewhat different than the next. The early and late treatment of cleft hand, therefore, has to be considered for each child. Late treatment in cleft hand is […]
Amniotic Constriction Band- how we can help function
Amniotic constriction band is a common condition which typically involves more than one extremity. While the belly and face can be involved in rare patients, the arms and legs are the classic sites. Every child with amniotic band is different. Totally. Sometimes, physicians refer to it as a syndrome but that is not really accurate- it is a random pattern of constriction rings, […]
Ulnar cleft hand, part II
My most recent post, from Dec 5th, was on a rare type of cleft hand, the ulnar cleft hand. Ulnar cleft hand is very different and even less common that the classic cleft hand which involves the central hand (classically with middle finger absence). There have been a few manuscripts on the topic of ulnar […]
Not the typical hand deficiency- ulnar cleft hand
A patient with a thumb and three normal fingers has a hand that functions at a near normal level and looks great. The narrow hand caused by a lack of a single finger (as long as the others are well aligned and no significant gaps exist) is not easily detected by others- it looks good. […]
Hand Camp 2019- St. Louis Shriners Hospital
I realize that I post about Hand Camp nearly every year. Our St. Louis Shriners Hand Camp is really something special. But I do so for good reason- it is just so impactful for kids, families, staff, and me! Being outside the hospital setting allows a different kind of conversation and allows a different perspective for […]
Nerve Injury after Trauma
The blog is mostly about kids born with differences in the arms (and occasionally legs). However, my practice also includes kids with sports injuries and other traumas. I will occasionally post interesting findings on these topics as well. This is a child with a nerve that is not working correctly after an elbow fracture. Specifically, […]
Activity Specific Prosthetics
This is a brief post on activity- specific prosthetics. There has been much controversy on the timing and appropriate use of prosthetics in kids. I have previously blogged about this several times as can be seen HERE. I really appreciate activity specific prosthetics. The child is engaged in the process based on a demonstrated interest and the specially […]
Untreated Adult Hypoplastic (Small) Thumb
On occasion, an adult comes to my clinic for evaluation of one issue and a previously unrecognized issue is identified. This type of presentation can come in different varieties and, due to my particular practice type, often we find a birth anomaly that has not been recognized or treated. This patient is one very interesting […]
Distal arthrogryposis, before and after
Distal arthrogryposis is very different from AMC or other forms of arthrogryposis. By definition, distal arthrogryposis includes joint tightness (contractures) in the hands and feet. Here is an excellent Link from NIH. I have also previous posted on distal arthrogryposis, those links can be found HERE. I wanted to share some early results on a 5 year […]
Fixators for Lengthening. Fun?
External fixators are devices that rest outside of the skin. They can be used to stabilize broken bones (although not used very often for this purpose today) or to correct a short or angled extremity/ bone. We use fixators to lengthen small bones such as the thumb to allow pinch or to grow the forearm […]
Forearm Synostosis
The forearm typically has two bones, a radius and an ulna. The benefit of having two bones is that it allows the radius to rotate around the ulna. This means we can position the hand palm up and down. This is functionally helpful but not functionally mandatory as there are many ways to make up […]
Only a thumb. Amazing outcome!
A child with a single digit may have one of two primary diagnoses. If there is a single digit– most resembling a little finger, the diagnosis is likely ulnar deficiency– most resembling a thumb, the diagnosis is symbrachydactyly Other diagnoses affecting the fingers include amniotic band syndrome which typically affects the central digits and causes […]
Severe Camptodactyly
Severe camptodactyly can be a challenge as it will limit function and may cause pain. This is less common in childhood and more common for the adult with untreated camptodactyly. I have previously shared thoughts on camptodactyly HERE. Treatment of camptodactyly in the child begins with therapy. Depending on the nature of the camptodactyly, this may […]
Distal Arthrogryposis- thoughts and techniques for treatment
Distal arthrogryposis is defined as multiple contractures affecting the hands and feet. This can include the thumb, fingers (camptodactyly) or clubfoot. Our understanding of these conditions continues to expand and these sites each provide great information:Rare Disease siteGenetics siteOMIM While distal arthrogryposis may be lumped as a diagnosis, the diagnosis can also be subdivided into […]
Short arm and hand deficiency- phocomelia or longitudinal deficiency?
Phocomelia is Greek for ‘seal limb’, a descriptive term for a short, deficient arm (or leg). I have previously posted on this topic HERE. For many years, patients with a really short arm were diagnosed with phocomelia as it became a ‘wastebasket’ term for such patients. However, the term should be used in patients with an […]
Symbrachydactyly- The typical form defined
I have posted a few times on symbrachydactyly and those posts can be found HERE. In addition, there are several reasonable summaries at other sites including this free ARTICLE from a friend and colleague, Michelle James. Many hospital sites also offer a brief summary of the diagnosis. In my practice, it is not common that patients come […]
Sprengel Deformity Outcome
Sprengel deformity is the presence of a high- riding shoulder blade (scapula). I have previously blogged about it HERE (although it has been awhile). Sprengel deformity is uncommon although the exact incidence is unclear. It can be associated with a number of conditions including Klippel Feil (cervical spine vertebrae fusions), scoliosis, and other less common conditions (although all […]
Research Matters
The Paul R. Manske Award for Best Congenital Manuscript is named for my late partner who had such an important impact on the field. This Award recognizes the most impactful paper related to kids born with hand or arm differences, anomalies, etc. I am happy to say that our paper was selected for this award […]
Finger Deformity- What happens late?
Clinodactyly, bent finger, may present at birth, in childhood, or with the rapid growth of adolescence. If the bent finger is mild, it will not limit function and often may be treated with stretching or simply observed. However, a more notable bent position becomes a functional issue with large object grasp and with simple things […]